A very ‘lively’ discussion is occurring between contributors of the blogging behemoth Science Based Medicine and Healthcare etc. I’ve been unable to register on SBM and this comment was too long for Healthcare etc so this is the comment I would have posted-
This is my contribution, I hope you don’t find it too inflammatory. I note that one of the more enlightened SBM cheerleaders on Dr Novella’s latest SBM post chose to demonstrate their non-arrogant non-paternalism by referring to Dr Zilberberg as a ‘dipsh*t’, so I should be on safe ground.
The SBM site won’t let me register, I’ve got an IT-savvy mate on the case but he’s had no luck, if I can crack it I’ll post this there too.
I had a bad feeling when this discussion began, when Dr Novella posted a response to Dr Zilberberg’s post. The risk was that only a ‘meta-discussion’ would ensue ie. a discussion disputing what had been discussed, how it had been discussed and how that reflected on the character of those discussing. This has been only partly true and kudos to Drs Novella and Zilberberg for their good faith in trying to understand each other.
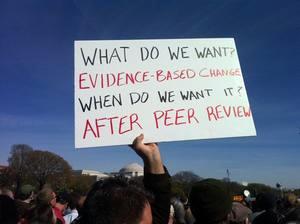
I don’t agree however that hotheaded arguing is always so bad; if progress is to be made in learning from each other’s positions I think taking a Popperian approach is more important than whether discussion is civil or intemperate. By which I mean trying to discuss concrete (falsifiable) points to arrive at a clear conclusion instead of quibbling over generalisations. For example the statement which was discussed, ‘absence of evidence is not evidence of absence’ may apply to a specific concrete instance such as a particular study not finding a new anticonvulsant to be effective due to small numbers/bias. The same statement may be used when discussing a different specific concrete instance such as 20 specific studies of homeopathy of which one shows benefit by p-value, with a different slant. Specific discussions about either application might be informative. I’m sorry but I’m not convinced that any abstraction beyond such specifics (short of a textbook on the philosophy of science) is informative, and I personally haven’t found the significance of this well-worn statement informatively addressed by either side in this discussion. This extends to other ‘points’ of discussion; there seems to have been a lot of talk about logic and illogic about positions which are not matters of logic. What I’m saying is it doesn’t matter how polite you are if you don’t stoop to discuss specifics.
Following from this I would bet my dear departed grandmother that if you saw Dr Novella, Orac, Dr Zilberberg or myself in clinical practice seeing real patients in the real world you would be hard pressed to say which was the arrogant paternalist and which the woo-collaborator. I bet across the board the practices would be competent and compassionate with a barely distinguishable difference in approach in the minority of cases where the patient raised CAM as an issue.
I don’t now plan to participate in idea-sharing in this discussion, I’ll explain why not in due course. I myself have an interest in individuals’ motives, I don’t know why, I just do. What follows may offend some but as above that’s ok, if you would like to insult me please come visit my blog, I could use the company.
On this note let’s turn to the SBM website. I was delighted when I discovered this gem, when I first came across Dr Attwood’s awesome series on the p-value fallacy and Bayesian analysis. I made the site my homepage and visited daily. I thought it would be a site discussing scientific debate and controversy within mainstream medicine; there’s plenty enough of that. Maybe the contributors would discuss, as Dr Attwood did, specific instances where the EBM hierarchy of study designs may inhibit critical thinking, a hobby horse issue of mine.
Instead I quickly became bored. Bored to tears. As it turned out SBM was actually mainly an anti-woo site. I’ve conducted an unscientific study of posts on SBM from September 1st to yesterday and I found of 41 posts (not including site business and humour), 24 posts (59%) were primarily anti-woo, 6 (15%) had a significant anti-woo element and 11 (27%) were not about woo at all. The non-woo posts were typically exceptional and very interesting, such as this and this.
To say I find the anti-woo posts boring is not to say that they’re unimportant or reflect poorly on their authors, it is just to say that I find them boring. I have no interest in CAM as it seems to me that deep knowledge about it and its invidious advocates is of little real help in the clinical practice of medicine. All this CAM talk doesn’t make one much of a better doctor.
Allow me to now go a bit arrogant and paternalistic. I know a bit about vaccines and vaccine refusal as well as whacky treatments for autism. I note that there’s now a pediatrician contributor on SBM and that he has authored many posts about vaccination (although the majority of posts about vaccination are not by him). For everyone else participating in this discussion I can safely say I’ve had more clinical experience dealing with vaccine-preventable disease and vaccine refusal in real patients than you’ve had hot breakfasts. I’ve seen babies die of pertussis, children maimed by pneumococcal meningitis, and more varicella than you could poke a stick at. (As an aside, the varicella and HPV vaccines are simply not as important as other vaccines and to imply otherwise is silly.)
What this clinical experience has taught me is the limited value or counter-productive effect of strong and emotive statements about CAM, and yes of arrogant paternalism. I’ve learnt the hard way what is the right approach to difficult CAM families where the stake is a child’s welfare not just blog point-scoring, and that approach is humble and inquisitive. I find these sorts of parents quite annoying but remind myself that the child is my patient, they are not. The humble inquisitive approach leads to real improved outcomes for real children. Bear with me here, I’m NOT accusing Dr Novella or anyone else of having the bedside manner of a paternalistic ass; I will return to this point.
Back to SBM. It seems to me that the word ‘science’ unavoidably contains a value statement, whether that is an appeal to authority or a statement about effective methods of reasoning. So it seems to me that those involved in a site with that name, which is actually primarily an anti-woo advocacy site, and not for example a site dedicated to hot controversies of the day within mainstream medicine, should not feel too victimised when their recruitment of the word ‘science’ within anti-woo discussions is considered by others to be largely an appeal to authority, and the site’s name largely a jab at CAM advocates (of whom I am no friend or ally).
All of which gets me thinking about motives. The statements that I object to most strongly in this discussion have been appeals to ‘ethical’ behaviour, to not acquiescing in the evil of CAM. When I hear ethics invoked in this way I reach for the lube. I simply don’t believe that these strong anti-CAM opinions have done a utilitarian good for society in this regard, though all the routine workaday medical care delivered by compassionate doctors for centuries, of which the authors are part, has. Here I am unscientifically generalising from my clinical experience as outlined above. I believe that it is most likely that the SBM site has had no overall remedial effect on the harms from CAM and it is quite possible that it has had a negative effect through alienating half-interested observers and galvanising CAM loons. I reject the assertion that the SBM site achieves a consumer protection mission. If you would like to shut me up you could point me to evidence of, for example, the increased vaccination rates attributable to these public opinion pieces or the imminent demise of the NNCAM.
This is not to criticise the act of blogging itself (I try not to be that hypocritical). It provides all sorts of good and is a lot of fun. In this discussion however I think it is fair to say that everyone’s real motives, including mine, have been the personal gains from the intellectual interest of the discussion itself and the personal gains of expressing one’s views to a sympathetic or antagonistic audience, not ensuring the best outcomes for our patients. For this reason I find appeals to ethics in bad faith and, ironically, the most paternalistic and arrogant statements in the discussion. If we all wanted to act as ethically as possible we would stop wasting our time with this ceaseless gasbagging and devote all our waking hours to even more mainstream medical research than we currently undertake, a choice which would indisputably provide a greater public good. In the meantime everyone should just chill out.